Sexual health challenges are common among people who have or had cancer. This is certainly true for cervical cancer, as treatment can affect sexual functioning in a number of ways, both physical and emotional.
It is understandable that for anyone dealing with cancer, the disease may take center stage. But it’s important to address sexual changes related to cancer as well. Sexual health is an important part of overall health and well-being.
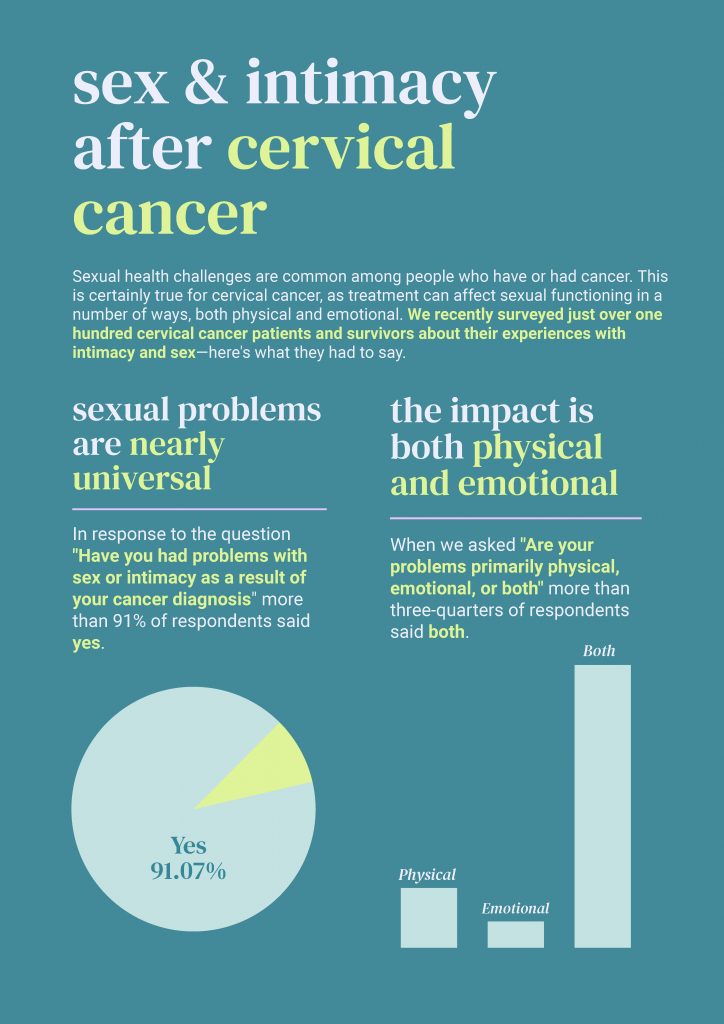
We recently surveyed just over one hundred cervical cancer patients and survivors about their experiences with intimacy and sex. Nearly all of them agreed that cancer has had an impact on their intimate relationships—and the problems are both physical and emotionalThe disruption can be significant. As one survey respondent commented, “This has had a massive impact. We are sexual beings and that loss is hard to accept.”
Types of Treatment and their Impact
Treatment for cervical cancer can bring about physical changes that in turn can make sex uncomfortable and less pleasurable. While there are ways to manage these physical changes, it helps to know what to expect.
- Radiation therapy can cause vaginal dryness or irritation making sex painful. It can also cause a condition called vaginal stenosis, where scar tissues forms in the vagina as a result of treatment. With this condition, the vagina becomes narrower and shorter, which, along with scarring, can also cause pain during or after penetrative sex.
- Chemotherapy side effects, like nausea and diarrhea, can lower interest in sex. Chemotherapy can also make vaginal stenosis worse.
- Surgical treatments can cause problems related to the type of surgery performed. Some women may have a hysterectomy, a surgery to remove the uterus. This may cause the vagina to become shorter and make sex uncomfortable. If the ovaries are also removed, menopause will start and bring with it various symptoms, including vaginal dryness. With less vaginal lubrication, vaginal itching, burning and pain during sex can result.
Treatment can also cause changes in self esteem and body image, and this can impact your sex drive. It cause difficulties in becoming aroused or achieving orgasm.
Managing the Effects of Treatment
Some types of problems that arise from treatment are easier to manage than others, but there are options to help address the physical challenges.
To help alleviate the symptoms of vaginal stenosis, women can use dilators—tubes made or plastic, rubber or silicone—to stretch the walls of the vagina and break down scar tissues. Kegel exercises can also help improve flexibility and strength. There are different options to treat vaginal dryness, including lubricants and vaginal moisturizers. Estrogen therapy may be appropriate for some women as well.
Finding the Support You Need
It can be a challenge to find the support you need. Even though sexual issues for cervical cancer patients are common, healthcare providers often don’t address them with patients. One study that found that only about 45% of all cancer patients had a conversation with their healthcare provider about sex—and men were much more likely to have the conversation than women. Our survey findings mirror the general findings of the study—45% of respondents said that they had successfully discussed these problems with sex and intimacy with a provider.
So more than half of cancer patients haven’t been able to get the support and information they need from a provider. The quotes below from respondents to our survey make clear that many patients struggle to have their concerns heard by their providers.

If your provider isn’t addressing your sexual health, keep looking! There are providers out there who will listen to your concerns and help find solutions. You can start with other providers on your care team—oncologists, nurses, social workers, and therapists all may be of help. But there are other ways to find resources:
- If you belong to a support group, you can ask for recommendations for a provider in your area.
- Check out local hospitals to see what programs exist for cancer patients and survivors, like the Sexual Health Program at the Dana Farber Institute, the Women’s Integrated Sexual Health Program at Ohio State University, or the Sexual Medicine & Women’s Health Program at Memorial Sloan Kettering Cancer Center.
- A certified menopause provider is trained to provide optimum menopause-related care, and will be well versed in managing symptoms such as vaginal dryness. The North American Menopause Society allows you to search for a certified provider in your area.
- You can also search for a certified sexuality counselor or therapist in your area.
Thoughts on Sex, Intimacy & Communication
See more from our survey of cervical cancer patients and survivors—download the infographic with survey results and links to resources that can help deal with sexual health challenges after cancer.
Additional Resources
- Manage Sex and Intimacy during and after Gynecologic Cancer Treatment: Information on how cancer treatments can affect how your body responds to sex, what you can do to have sex that is safe and feels good, and when to get medical help.
- Staying Close through Cancer: In this article from Cancer Today, experts who address sexual function emphasize that cancer doesn’t have to mean the end of sex or have a negative impact on relationships.
- Women’s Guide to Sexuality During & After Cancer Treatment: A resource from Oncolink offering tips for sexual activity and dealing with vaginal changes.
- Self Image and Sexuality and Sexual Health Issues in Women with Cancer, resources from the National Cancer Institute.